Why Looking After Your Smile May Prolong Your Life
Table of Contents
Can you guess what mouth disease this is?
- Most people experience it more than once,
- Is much less common in children,
- Affects 3 out of every 4 adults in the UK,
- More than half of teenagers have some form of the disease,
- Is the leading cause of tooth loss in adults
Is it
- Tooth decay?
- Halitosis?
- Misaligned teeth?
- Gum disease?
The answer to the question is gum disease (gingivitis). And contrary to what people believe about tooth decay, the most prevalent oral disease in adults is gum disease.
What is Gingivitis or Gum Disease?
Gum disease, also known as gingivitis, is an inflammation of the gums that can progress to affect the bone that surrounds and supports your teeth.
What Causes Gum Disease?
Gum disease begins when naturally-occurring bacteria in your mouth interact with plaque, that sticky deposit that forms in your teeth after you eat or drink, releasing various chemical compounds that trigger an inflammatory response in the gum.
As bacterial colonies grow and more plaque forms, the inflammatory reaction from the gum becomes more and more pronounced. Net result? The tissue in the tooth socket begins to disintegrate and the tooth becomes lose.
Risk Factors for Gingivitis
There are many risk factors associated with the gingivitis, such as
- The tar deposits on the teeth of a smoker act as magnets for plaque and bacteria. Smoking is also known to lower the chances of successful treatment.
- Hormonal changes in girls/women. Changes during ovulation, menstrual cycle, or pregnancy, are known to make gums more sensitive and make it easier for gingivitis to develop.
- People suffering from diabetes have a higher risk of developing infections, including gum disease.
- Other illnesses. Diseases that compromise the normal functioning of the immune system can also affect the health of gums.
- Medical treatments. Some cancer treatments, medications for transplant patients, medications intended to reduce the production and flow of saliva, can all potentially increase the risk of developing the disease.
- Inadequate plaque control. Partial dentures, poorly fitting crowns, veneers and orthodontic treatments such as braces can become reservoirs of unwanted plaque deposits, in cases where patients’ plaque control is inappropriate.
- Genetic susceptibility. Some people are more prone to severe gum disease than others.
What are the early symptoms of Gingivitis?
In the early stage of gingivitis, your gums might swell and bleed. Early signs of the disease include
- change in colour of your gum line (from pale pink to red or purple)
- gum bleeds easily when you gently poke it (with an interdental brush, for example) or when you brush your teeth.
How is Gingivitis Treated?
Alarming as it might be, seeing blood when you brush your teeth is actually a sign that your organism is already fighting the disease. The important thing here is to act quickly at the first sign of blood. The good news is that in its early stages, gingivitis can be reversed in nearly all cases. The bad news is that your body cannot win that war against gingivitis on its own. A proper plaque control regime is required to stop the swelling and restore your gums to a healthy state.
If Gingivitis persists for more than 2 weeks you will need to visit a dentist for treatment. Depending on the severity of the gingivitis treatment options will include;
Deep Cleaning
Deep cleaning techniques include scaling, root planning and laser removal.
Your dentist will first scrub and remove plaque and tartar from your teeth, gum pockets and gum line. Then antibacterial mouth wash will be squeezed into the gum line to aid cleaning. Additionally Root planing is used to remove infected sections of your teeth and smooth any rough areas that may be aggravating your gums. This simple treatment will take place over a minimum of two sessions and, combined with a proper brushing, flossing and cleaning routine will cure most cases of gingivitis.
In addition a range of medications can be used to help treat gingivitis.
The most common treatments are antibiotic mouthwashes. These mouthwashes use disinfectants to help keep gums and teeth clean – allowing the mouth to heal efficiently. Additionally antiseptic and antibiotic treatments can be inserted directly into gum pockets to keep problem areas clean.
However, in severe cases of gingivitis surgery may be required. This usually is only necessary after gingivitis has been left untreated for a considerable period.
Flap surgery is a treatment that cuts into the gums to allow access to deep plaque pockets. These pockets are then cleaned thoroughly before the flap is sutured closed. This creates a better fit for the gum and should prevent recursion after healing.
Bone and tissue grafts are treatments where bone and tissue is added to the gum line in order to restructure the area. This treatment becomes necessary when gingivitis has damaged the gums and teeth so severely that reconstruction is required to prevent further problems.
Once initial treatments have been completed strict plaque control regimes that include flossing, brushing, mouthwash and rinsing regularly are usually all it takes to prevent the recursion of gingivitis.
Complications of Gingivitis
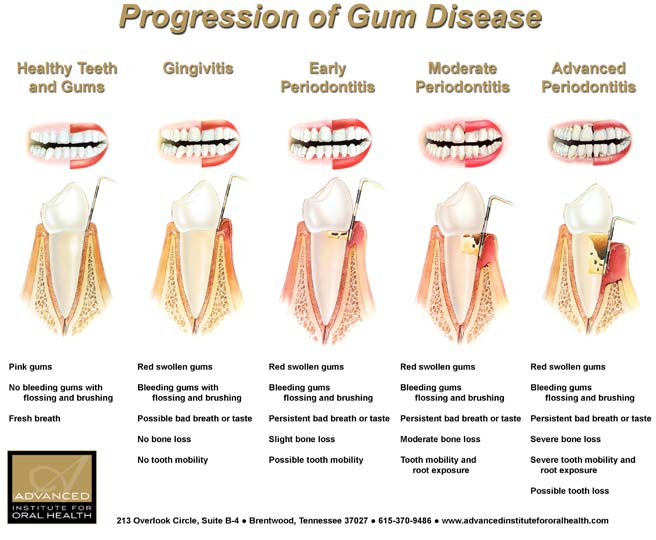
Left to progress, gingivitis quickly turns into a more severe stage of gum disease known as periodontitis (which literally means ‘inflammation of the area around the tooth’) and periodontal disease.
During this severe stage, the gums detach from the tooth creating pockets where more food, detritus, calculus and bacteria can grow. As the deposits grow in these pockets, the body’s immune system kicks in and starts fighting the bacteria. The bacterial compounds and the body’s natural response to infection start to literally dissolve the bone and connective tissue that hold teeth in place. Damage quickly spreads from the gum, to the bone and to the root of the tooth, until eventually the tooth falls off.
Can Gum Disease Cause Health Problems Beyond the Mouth?
Although gum disease on its own is not life-threatening, there are a significant number of studies that indicate that the disease might be a contributing factor to conditions such as heart disease, heart attacks, stroke, and rheumatoid arthritis. Other studies have shown that diabetics who suffer from gum disease might find it more difficult to control their blood sugar. And there has been some research that suggests there may be a tie between poor oral health and an increased risk of dementia.
How Can I Keep my Teeth and Gums Healthy?
Advances in technology and formulations mean that today we all have access to mouthwashes and electric toothbrushes that can help in bring the disease under control. Some studies have shown that the regular use of mouthwash can reduce the risk of gum disease by more than 50 percent. It is important to use a mouthwash that contains fluoride. Likewise, more and more evidence suggests that electric toothbrushes could be more beneficial than manual ones when it comes to preventing the onset of gum disease, simply because they are more efficient at helping rid the teeth of debris. Flossing is also essential to stop pockets of plaque building up along the gum line.
However, the most important tool in your arsenal for plaque control is to ensure that you visit your dentist at least twice a year. Research has shown that tooth loss is more common in people who fail to see their dentist at regular intervals. Finding a dentist you can trust can be a difficult task. Many services, such as What Clinic can be a great resource of information and reviews of dentists available in your area.
Here’s to a healthy smile and a long, happy life!