A viral liver disorder, hepatitis C is considered the most common disease transmitted through the blood in the US. This blood borne ailment is difficult to detect; many Hep C patients do not even realize they have it. This disease advances through contact with infected patients and is primarily the result of using injectable drugs. Immunizations exist against other forms of hepatitis. However, HCV does not have any vaccination associated with it. In case the virus is not cured within half a year, it turns into a chronic infection only curable with medication. HCV also causes scarring, liver cancer, cirrhosis and even death. Some new medications have come about for curing this chronic viral infection. About 3.9 million US residents have this disease. Many are unaware they even suffer from HCV. The hepatitis C virus causes infection. An inflammation of the liver due to virus, this disease spreads or transmits when the person comes into contact with infectious fluids and secretions from those infected by the hep C virus.
Hepatitis C is characterized most commonly by muscle ache, fatigue, yellow tinge in the eyes and skin, tenderness in the upper abdomen and dark colored urinary discharge. Light coloring of bowel movements is also noted in HCV patients. This contagious disease can be transmitted across people, through not just blood but other body fluids that also contain the infected person’s blood. For those sharing injectable drug needs with infected persons, HCV can be a real threat.
Diagnosed through medical history and understanding of the extent of exposure to the infected person, HCV can also be detected through pathology reports, exams and positive blood testing. Usually, the disease can be cured by antiviral drugs prescribed by HCV specialists. These drugs are not your average antibiotic. Considering there is no vaccination for this disease, treatment is the only means of countering it. Of those who suffer from hepatitis C, around 15-25 percent are infected patient who spontaneously recover while others become chronically and persistently infected. Through early treatment and diagnosis, the prognosis is positive for those who become chronically infected. Untreated hepatitis can be prevented by avoiding blood and bodily fluid contact with infected individuals. However, there can be severe complications if the disease is not detected and treated at initial stages including liver failure, cirrhosis, liver cancer, need for liver transplants and death.
As it is tough for individuals to get rid of hep C from the human body, this disease is widely prevalent across communities, especially with chronic infection. At the time the virus first comes into the human body, there are very few to zero symptoms to detection is also difficult. The Center for Disease Control estimates that 29,718 new HCV cases were reported in 2013. With more than 3 million in the US chronically infected by this disease, precaution is a must. Infection is most common among those 40-60-year-olds. HCV disease also leads to at least 8 to 10 thousand deaths per year in the USA. It also is the prime cause for liver transplants in the US and implicated in the etiology of cancer of the liver.
Symptoms of Hepatitis C
Table of Contents
Early Stages
Many individuals with HCV do not report any symptoms at an early stage. Those who do may report lack of hunger, pain in the muscle and the joints, tiredness and fatigue, nausea and vomit and abdominal pain. Hepatitis is the inflammation caused in the liver and there are six different strains of this infectious disease ranging from one to six. The most common hep C disease in the US is genotype number one. There are some variations within it as well. Genotypes 1a/1b for instance. Some viral strains of HCV respond more to management and medication than others.
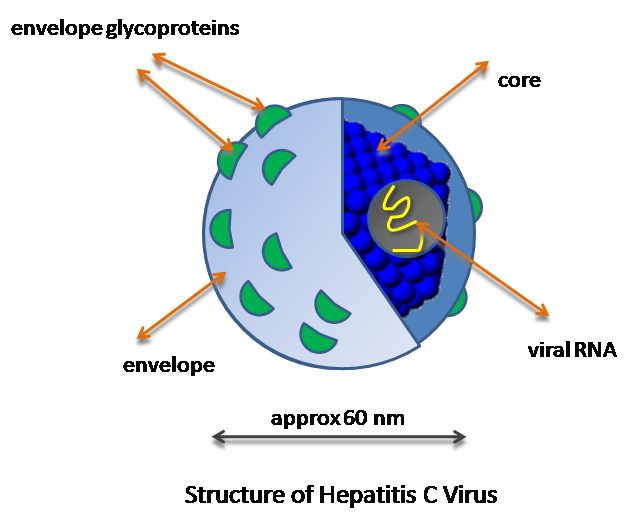
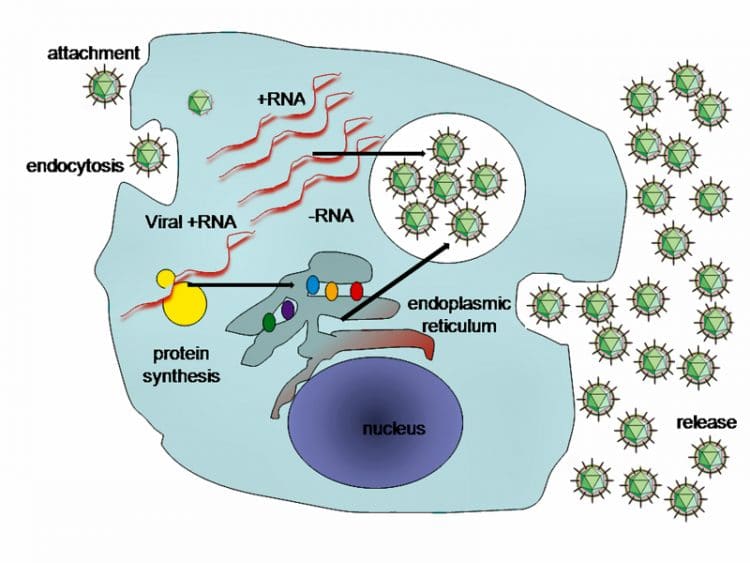
Much like any other human-immunodeficiency viral infection, Hep C is known to advance very rapidly and grow prolifically in the human body. These genes make the surface proteins in the virus pathogen also transition fast. Around 1000s of genetic variants are produced every day. The body cannot keep up with HCV antibodies against a whole range of these at one go. Therefore, it is not even possible to develop a vaccine for this disease.
It essentially impacts the immune system which in turn, causes inflammation. Acute and/or early stages of infection are characterized by clay-colored discharge and dark urine. Chronic and advanced forms of this disease display symptoms only at a later stage. This is why HCV is counted as an insidious disease. Over a span of years, or even decades, the long standing inflammation causes liver cell death and scarring or fibrosis. Advanced scarring of the human liver is known as cirrhosis. This impairs vital liver functions as well and creates susceptibility to liver carcinoma or hepatoma. Consuming alcohol further speeds up the symptoms of this disease. HIV infection alongside also aggravates cirrhosis of the liver.
While as many as 75% of the sufferers may lack symptomatology when they first get HCV infections, the rest may suffer from the preliminary symptoms. Fewer people experience Hep C symptoms such as yellowness of the eyes, dark colored urinary discharge or clay- colored stool. Infected persons also become tired or complain of certain symptoms as liver cirrhosis grows.
Later Stages
Raised liver enzymes occurring in the blood, apart from fatigue and/or weakness. happens later Loss of hunger and weight result, and in males, gynecomastia or breast enlargement may result. There is also redness of the hand palms and problems in blood clotting. Additional symptoms at this stage case spidery blood vessel growth on the skin. There is a pain in the abs and blood from the esophagal area. Fluid also collects in the abdomen. During later stages, jaundice symptoms may appear along with confusion and lack of focus. The person can even slip into a coma.
As the disease is transmitted via the blood, no contagion period is there as such. Those with chronic forms of this disease can be contagious until they are cured. This disease is caused by blood borne pathogens and those infected may report GI symptoms within 6-10 weeks post the initial infection. HCV can also be passed to the unborn child by the mother, with 4 percent of children born with this disease from infected mothers. Hep C is not transmitted by the breast milk, however.
A certain type of HCV virus is also caused by intercourse. Infected individuals can pass on the disease to partners and spouses at the rate of 1 to 4 percent. Hep C is not transmitted by causal touch or sharing of utensils, sneezing, coughing or even close contact. Infection control can also be compromised in those individuals with tattoo or body piercings who have shared needles. Organ donors can also transmit this disease.
Most signs and symptoms of the HCV virus pertain to the liver. But the disease can impact organs other than this as well. Hep C can cause pathological antibodies like cryoglobulins which lead to inflammation of the arteries through vasculitis. This causes damage to the joint, skin and kidneys as well. It also leads to arthritis, general pain, water retention or inflammation and purple colored leg rash.
Individuals with cryoglobulinemia also have Raynaud’s phenomenon in which toes and fingers turn form white to purple and then red. These parts also become painful when the temperature dips.
Two Stages of HCV
There are two stages of hep C. The acute or early phase occurs soon post the infection. Most individuals lack symptoms at this stage. Around 75-85 percent of individuals infected by this disease can become chronic cases. At the chronic stage, there may be a lack of symptoms for years at an end. Multiple subtypes of Hep C abound. These are differentiated on the basis of medication used, dosing and therapy duration.
Some of the symptoms that may result include easy bruising and bleeding at later stages. Slurred speech, confusion, drowsiness, and skin itching or joint pain may also result. As other forms like Hep A and B also exhibit similar symptoms, blood testing is essential to diagnosis HCV.
In the acute stage, 2/3rd of the individuals who become infected lack symptoms. For those developing symptoms 2-24 weeks post the infection, the symptoms may last for this period. Upper ab pain, jaundice, nausea and upset stomach, low-grade chills, and fever, as well as fatigue, are common during this stage. Additionally, there are mood swings and itching of the skin as well.
Complications of HCV
These can be serious to moderately life-threatening and include liver damage and cirrhosis. More complicated outcomes include liver failure, liver carcinoma, and death. Acute HCV infection is diagnosed with definitive symptoms. It is called a silent epidemic as well. Average time frame from the infection to the symptoms can be between 15 to 4 weeks.
At the acute period, symptoms will not appear different as opposed to those caused by viral syndromes. Those with acute HCV experience ab discomfort, joint pain and more. As HCV becomes chronic, the virus remains in the blood for as long as 6 months post the acute-infection phase. In case the presence of HCV viruses is detected twice over the period, a chronic diagnosis confirmation is given. The infection will only be resolved when treated using medication.
While most people experience a lack of symptoms with chronic HCV, persistent fatigue, aching joints, and ab pain are also possible. After a long period of 25-30 years, chronic infection results in massive scarring or liver fibrosis. If the entire liver undergoes scarring, this can cause cirrhosis, failure and liver cancer. The overall health of infected persons and their liver determines how the disease will advance. The genotype of the HCV plays a lesser role in the manifestation of symptoms. Only when the liver is about to collapse, does the infection become visible in many cases?
The symptoms and physical changes occur in case a liver failure occurs. It no longer has functionality such as removing toxins from the blood, fending off infection, metabolizing drugs, generating critical proteins, manufacturing factors for blood clotting and storing fat, vitamin, mineral, and sugar for use in the body.
Causes of HCV
HCV can result from a variety of reasons. Many drug addicts or users who inject or snort drugs can be susceptible to this disease. Additionally, those with persistent ALT levels, or alanine aminotransferase is a liver enzyme located in the blood can suffer from HCV. Those with HIV infection or those born to HCV or HIV positive mothers can also suffer from this infectious disease. Those on a long-term hemodialysis or tattoo in unregulated settings such as prison or by a person not licensed. Susceptible to this disease are those who got clotting factor produced before 1987. Those who have received transfusions or organ transplants before July 1992 or were notified they received blood from donors tested positive for HCV can also develop this disease. Following an accidental needle stick, health care professionals, emergency medical and public safety workers can also suffer this disease. Another source of exposure is eye or mouth exposure to blood of the infected individual. Those exposed to HCV should be tested for the viral RNA loading within 6 months, rather than testing for antibodies which may emerge only at a later stage in the HCV infection.
Yearly screening is critical for those with ongoing risk factors like STDs or those with multiple sex partners. Ongoing IV drug usage, long-term infected partners can also be risk factors.
Who Should Be Tested for HCV?
Hepatitis C is a liver inflammation caused by virus-like HCV. The word is derived from hepat which means liver and itis which means inflammation. The Center for Disease Control holds that disease testing is essential for those who receive blood from donors with the disease, those injecting drugs, organ transplants or blood transfusion before July 1992 and a blood product used to treat clotting problems prior to 1987. Also, those born between 1945 and 1965, have been on long-term kidney dialysis and were either born to an HCV or HIV positive mother. Those with HIV and symptoms of liver disease should also be tested for it. Transferred to the blood by intravenous drug use, unsafe sex or contact with body secretions or blood, this HCV virus is preventable if safety is followed.
The liver is responsible for functions such as bilirubin removal, conversion of ammonia to urea, immunity factor, cholesterol and bile management, storage and release of glucose and storage of iron. HCV affects a lot of people and is a tough virus which can live for up to 3 weeks on surfaces at room temperature. It is contagious and spread by blood transmission.
HCV occurs when the liver undergoes inflammation due to excessive alcohol, infection, disease, poisons or drugs. Needle or syringe sharing, material child transmission, accidental needle sticks, sharing brushes or razors or multiple partners and tattoos or body piercing can increase the rate of risk as well. Prior to 1990, blood transfusions were also a cause of HCV. Now all blood transfusions are checked for HCV virus.
An uncommon mode of transmission is through transplantation of the organ from an infected HCV patient. The use of HCV positive organs is only for advanced cases of life-threatening nature.
HCV has also been associated with hemodialysis used to clean the blood in end stages of a kidney disease. Infection and sterilization of equipment are essential. Those with hemophilia are also prone to this disease.
Treatment
HCV treatment is only possible through effective tests, diagnosis and medication. Often assumed to be flu in the early stages, this infection is rarely diagnosed during the early acute stage. Immunity of the person with HCV can be impacted in only 20% of the cases and the remaining 80% turn chronic, spreading HCV infections to others without their knowledge. Screening tests are available as well as simple blood tests. A US FDA approved test provides results in 20 minutes. The blood is drawn from the vein and processed at the lab. A negative test means lack fo exposure. But a positive test only indicates exposure and not necessarily infection. Positive HCV antibodies can be detected through the RNA or PCR test which assesses if the virus is still present. Persons with positive PCR results need to see an HCV specialist. Once chronic infection is detected, the genotype is assessed through testing. This determines the the extent of risk and the future direction of medication.
Medication
The present treatment for chronic hep C is a blend of medications. Genotype 1a is the most prevalent in the US and requires treatment using a combination of powerful antiviral medicines. Direct acting antivirals are the newest class of medication that prevent the replication of the HCV viral cells. Before DAA, the cure for this disease was lengthy, tough and had a less than ideal prognosis. Now the cure rates are well over ninety percent. The average duration of treatment of 8-12 weeks The medicines are well tolerated and common side effects are fatigue and headache.
Treatment for HCV depends on viral load, genotype or strain, nature of the liver damage and other health conditions. A lot of people have acute hepatitis C infection and do not know they have a virus and do not opt for treatment, therefore. If the person has been exposed to the virus, early medication may be possible. Milder treatment options like bed rest, a healthy diet and zero alcohol are offered. Chronic hep C lasts for 6 or more months, and if you have scarring of the liver, anti-virus medication is recommended.
In August 2017, FDA approved pibrentasvir and glecapravir combination called Mavyret. Mavyret offers less cycle of treatment of only 8 weeks. It is for those without liver scarring or previous instances of HCV. Those at advanced stages of the disease need to have prescribed dosage of 3 tablets of potent anti viral medicines daily.
Once during the day medicines are also there like Zepatier and Harvoni. While the former combines elbasvir and grazoprevir, the later blends sofosbuvir and ledipasvir. Vosevi is a combination of voxilaprevir, velpatasvir and sofosbuvir. It is for those with chronic HCV, with or without cirrhosis who have received treatment. A combination of Olysio or Sovaldi with peginterferon taken daily by injection and ribavirin coming as tablet, capsule or liquid can be used.
Interferon and ribavirin are used for curing hep C too. They do have side effects like depression, anxiety, anemia, skin rash, and flu type symptoms. The most common types of chronic hep can be cured.
Blood Tests
There are numerous blood tests for antibody to hep C. It is taken for up to 6 months for antibodies after initial infection with hep C. if the antibody test is positive, several tests can be used to detect the viral load or identify the genotype of HCV.
Liver Biopsy and Non-Invasive Tests
The next step is to check the scarring of the liver. A liver biopsy involves testing liver tissue under a microscope. Noninvasive tests like liver stiffness and transient elastography can also be used.
Medicines for Different Genotypes
For Genotype 1, daklinza, epclusa, harvoni, and olysio as well as viekira pak are recommended. Also used are zepteier and viekira XR. Genotype 2 requires treatment with Epclusa and Sovaldi plus ribavirin. For Genotype 3, the drugs used are daklinza with sovaldi, Epclusa, and Sovaldi plus ribavirin. For treating Genotype 4, the recommended medicines are epclusa, harvoni (sometimes coupled with ribivarin), sovaldi plus ribavarin. Technivie plus ribavarin and zepatier are also given, the latter sometimes used with ribavarin. For Genotype 5, the drugs used are Epclusa, adnd Harvoni. For the final genotype too, Genotype 6, the same medicines are given.
Currently, DAA drugs used are simeprevir, ombitasvir, dasabuvir, sofosbuvir, ledipasvir, paritaprevir and some of these used in fixed combination drug forms are Technivie, VIekiria Pak, Harvoni, Mavyret, Zepatier, and Epclusa.
Conclusion
While regular screening for HCV is important, the treatment should also be prompt. In the ultimate analysis, prevention is possible only if precautions are taken. For the HCV sufferer, prompt treatment is of utmost importance to prevent further complications. Get yourself tested and stay safe, especially if you meet the risk criteria outlined by the CDC.