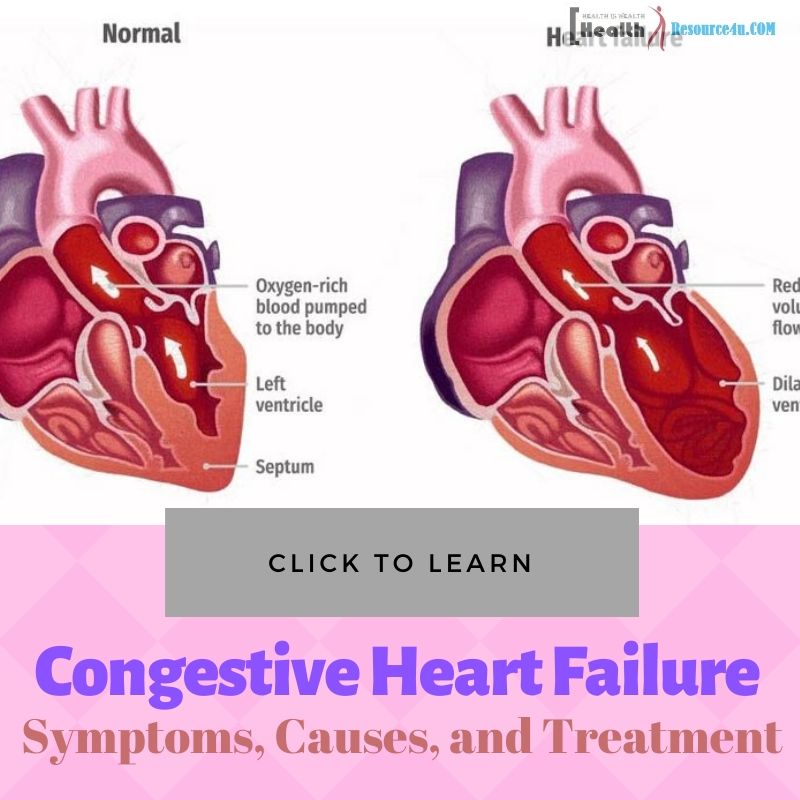
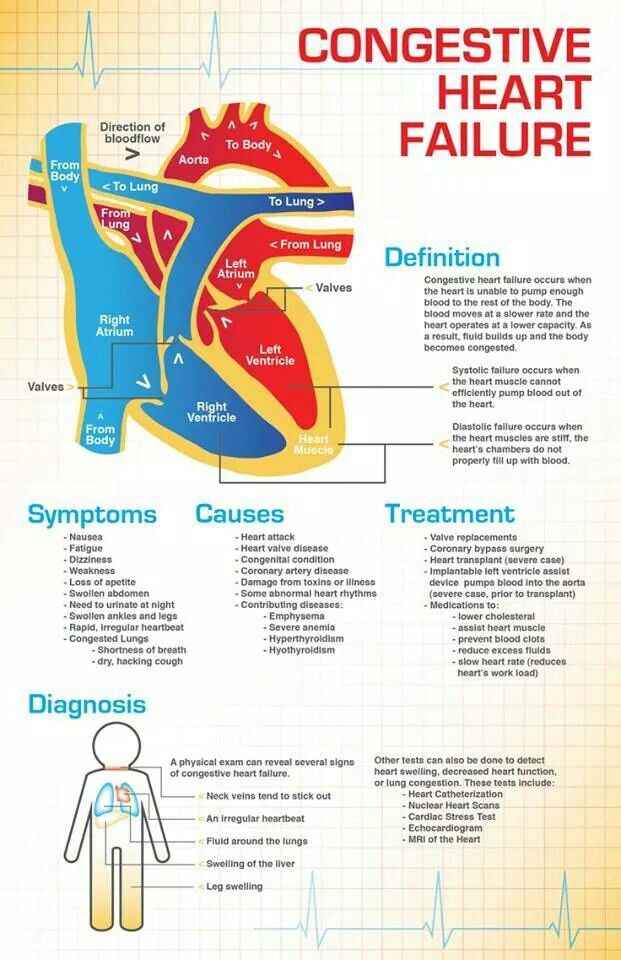
Congestive heart failure is a disease characterized by the heart’s inability to effectively pump blood throughout the body. In most cases, congestive heart failure occurs when other illnesses or conditions weaken the heart, leaving it unable to function effectively. This illnesses is associated with a variety of symptoms, and is often treated with a variety of medications and medical approaches. The following is an-depth look at congestive heart failure, which includes information on symptoms, causes, treatment options and more.
Symptoms
Table of Contents
The effects of congestive heart failure can be either acute or chronic, and typically involve signs and symptoms like the following:
- Chest pain, especially when heart failure is the result of a heart attack.
- Swelling in the extremities, especially the feet, ankles and legs.
- Shortness of breath. This symptoms can coincide with physical exertion, but may also occur when the patient lies down.
- Irregular or rapid heartbeat.
- Persistent cough. In some cases, coughing may produce phlegm, which is often foamy, frothy and/or tinged with blood.
- High blood pressure.
- Decreased energy, physical weakness and fatigue.
- Weight gain
- Swelling in the abdominal area, which is the result of fluid retention.
- Frequent urination, especially at night.
- Decreased appetite.
- Nausea or vomiting.
- Difficulties focusing or concentrating.
Causes
Illnesses and conditions like the following can contribute to the development of congestive heart failure:
Coronary artery disease
The most common cause of congestive heart failure, coronary artery disease is associated with a narrowing of the arteries, which weakens the heart and leaves parts of the body deprived of oxygen-rich blood.
Heart attack
When a heart attack occurs, the heart is often permanently damaged. This damage leads to poor cardiac function, which may result in congestive heart failure.
High blood pressure
Blood pressure is measured by the force at which the heart pumps blood through the arteries. The higher the blood pressure, the harder the heart must work to effectively supply the body with blood. Over time, this weakens the heart and arteries, which can result in heart failure.
Myocarditis
This complication is typically caused by a virus, and may lead to failure in the left side of the heart.
Heart arrhythmias
Abnormal heart rhythms can weaken the heart by causing it to beat too fast or too slowly, both of which can eventually result in congestive heart failure.
Other causes.
A variety of illnesses can lead to decreased heart function. These include, but are not limited to, diabetes, emphysema and thyroid disorders, as well as both viral and bacterial infections.
Medications Used to Treat Heart Failure
Because heart failure is a chronic condition, it often requires the lifelong use of medications. However, with the right drugs and self-care methods, cardiac function may improve, which can reduce symptoms, prevent complications and enhance overall health and quality of life. And while prescribed medications can vary on an individual basis, the following drugs are often used in the treatment of congestive heart failure:
- Beta blockers. These medications reduce blood pressure, slow heart rate and can even repair and reverse heart damage.
- ACE inhibitors. ACE (or angiotensin-converting enzyme) inhibitors can widen the blood vessels, lower blood pressure and reduce strain to the heart.
- Angiotensin II receptor blockers. Like ACE inhibitors, these medications enhance heart function by widening blood vessels and reducing blood pressure.
- Inotropes. In severe cases, these drugs are administered intravenously, and can regulate blood pressure and improve cardiac function.
- Diuretics. Diuretics help the body rid itself of excess fluids. In patients with congestive heart failure, these medications can reduce the amount of fluid buildup in the lungs, which can improve both respiratory and cardiac function.
- Digoxin. This drug, often called digitalis, can reduce heart rate and strengthen the heart’s muscle contractions.
Procedures and Devices Used in the Treatment of Heart Failure
A number of surgical procedures can be used to reduce the symptoms of heart failure, some of which include the following:
- Bypass surgery. When heart failure is the result of blocked arteries, coronary bypass surgery can improve heart function. During these procedures, blocked arteries are bypassed via blood vessels in the chest, arms or legs, thus promoting healthier blood flow through the heart.
- Heart valve repair. If a faulty valve is a contributing factor of heart failure, a surgeon may recommend that the valve be repaired or replaced. Some valve repair procedures are minimally invasive, while others require open heart surgery.
- Implantable cardioverter-defibrillators, or ICD’s. These devices are implanted beneath the skin, and are used to monitor heart rhythms and, if necessary, correct arrhythmias.
- Pacemakers. These implanted devices deliver electrical impulses to the heart’s lower ventricles, which helps them pump more efficiently.
- Transplants. When medication and other approaches aren’t effective in reducing symptoms and improving cardiac function, heart transplant surgeries are often necessary.
End of Life Care
Even with the proper treatment, heart failure may often progress to the point where it necessitates end of life care. This type of treatment, also called hospice care, is designed to provide the patient with physical, psychological and emotional support, and can be administered either in the patient’s home or in a medical facility. Typically, hospice workers provide a number of services, including medical treatment, help with grooming, psychological counseling and other integrative therapies. Some companies also offer a number of educational and emotional support services for family members and caregivers, as well as financial consultations and more. According to Jill Mendlen, registered nurse and founder of San Diego hospice, LightBridge, end of life care is designed to provide patients with strength, hope and comfort, in addition to personalized, professional care.
Lifestyle Choices and Self-Care
A number of lifestyle changes can help relieve symptoms of heart failure, as well as improve heart function and prevent complications. A few healthy changes include those listed below:
- Don’t smoke.
- Don’t consume alcohol in excess.
- Lose weight or maintain a healthy weight and body mass index.
- Restrict salt, cholesterol and fats in your diet.
- Get moderate exercise, three or more times per week.
- Avoid stress and stressful situations.
- Get enough sleep.
Prevention
In order to prevent heart failure, measures must be taken to eliminate the contributing factors of this disease. For example, a healthy lifestyle, combined with techniques to manage other heart-related illnesses, can significantly reduce a patient’s risk of developing heart failure.