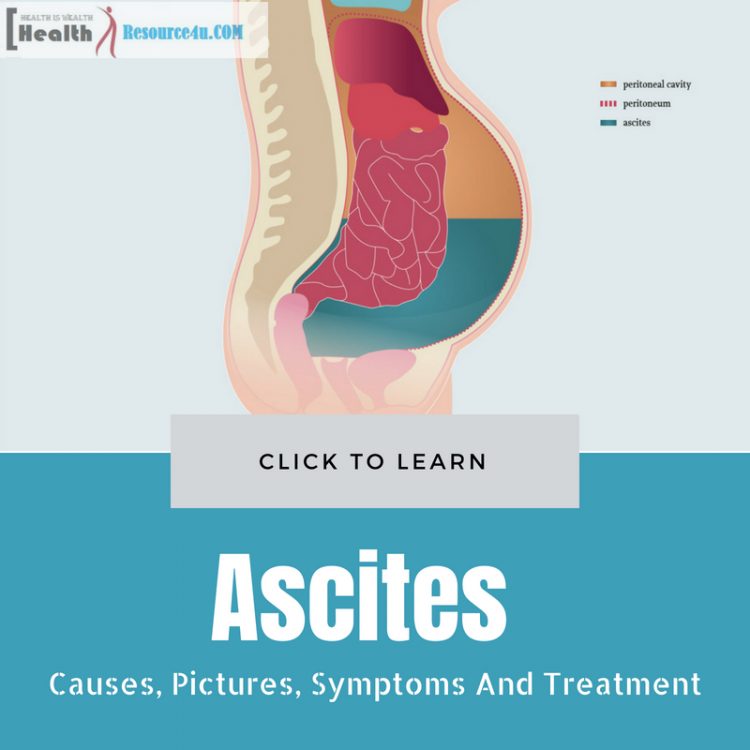
Ascites refers to a condition when there is increased fluid in the peritoneal cavity. So, what’s this cavity about, and where is it located? Well, the abdominal organs are contained in a sac/membrane referred to as peritoneum. This peritoneal cavity generally includes a low amount of fluid (though it varies in females by 20 milliliters or smaller than an ounce), based on the menstrual cycle. Ascites is a disorder when fluid levels are abnormal.
So many different diseases can trigger fluid accumulation. Therefore, the signs, symptoms, and complications of ascites depend on the condition, which is the underlying cause for it. Cancer spreading to the peritoneal cavity causes direct fluid leakage, even as other illnesses cause sodium and water accumulation in the body. Such fluids enter the peritoneal cavity in this condition.
In most cases, ascites results from liver disease. The liver is unable to generate enough protein to retain fluid in the bloodstream and obstructs the flow through scarring of liver cirrhosis. Oncotic pressure holds the water in the bloodstream. But in this disease, the protein pulls water molecules from leakage onto the surrounding tissues from blood vessels’ capillaries.
When the liver disease advances, the liver’s capacity to manufacture proteins diminishes, as a result of which oncotic pressure falls because of a lack of protein in the human body. Water comes into the adjacent tissues. Along with the critical ascites symptoms of fluid buildup in the abs, extra fluid can spread to other body parts. Edema occurs in a variety of organs such as feet, legs, chest cavity, and lungs. Symptoms due to excessive fluid are based on the location. Ascites causes a fluid buildup which triggers swellings and inflammations in a matter of days. The disease itself is painful to bear, causing nausea, breathlessness, tiredness, and a sense of being full.
While liver disease is a common ascites cause, cancer and heart failure can also trigger this medical condition. So the condition is a symptom of an underlying chronic condition. Swelling and weight gain are typical features. Prognosis and outlook for patients depend entirely on the severity of the disease. By measuring the stomach girth and monitoring weight, this disease can be regulated.
Causes
Table of Contents
Ascites occurs when there is abdominal fluid accumulation. This accumulation takes place between the membrane layers making up the peritoneum, a body organ smooth sac. Small amounts of fluid in this cavity are fine, but when fluid builds up, this disorder occurs. Many underlying medical diseases can cause this condition. It ranges from TB to pancreatitis, hypothyroidism, and TB. The most well-known causes of ascites are heart failure, cancer, and of course, liver cirrhosis.
Cancer can cause this condition when it impacts the following body parts:
- Lymphatic system
- Liver
- Peritoneum
- Ovaries
- Breast
- Gut
- Bowel
- Womb
- Pancreas
- Lung
Liver Cirrhosis
However, the most common reason for ascites remains liver cirrhosis of an advanced stage. This condition is an advanced liver disease, whereby experts suggest portal hypertension is the critical factor. Portal hypertension refers to the increased pressure of the blood flow to the liver. The essential principle is akin to the edema formation elsewhere in the human body due to differences in pressure between the inside circulatory system or high-pressure system, and the outside, low-pressure space of the abdominal cavity. A decrease in blood marks an increase in portal blood pressure carried protein albumin. This reason could be why there’s a pressure gradient resulting in ascites. The exact mechanisms of causation are still being explored.
Kidney Disease
Still, other factors such as water or salt retention can also lead to ascites. Circulation of blood volume may be seen as less by kidney sensors. This is because ascites formation depletes blood volumes. So, the kidney attempts to reabsorb excess salt and water to compensate for the volume loss. Specific causes of the disorder related to the high-pressure gradient, namely advanced kidney failure and congestive heart failure on account of generalized body fluid retention.
Budd-Chiari Syndrome
In rare cases, increased portal system pressures can also result from obstruction of the portal vessel either internally or externally. This leads to portal hypertension sans cirrhosis. Instances of this can range across tumor or mass pressing on the portal vessel from within the abdominal cavity or resulting blood clot formation in portal vessels obstructing the normal flow, and increasing vessel pressure. The cause for this occurrence can also be the Budd-Chiari syndrome.
Malignant Ascites
Malignant ascites can occur due to different types of cancers like ovarian, lung, pancreas, colon, lymphoma, or breast cancer.
Pancreatic Ascites
Further, pancreatic ascites can be seen in those with chronic pancreatitis or pancreas inflammation. Common causes of chronic pancreatitis are extensive alcohol abuse. This condition can also result due to pancreatic trauma and acute pancreatitis. Even diseases like tuberculosis which affect the abdominal lining can cause this condition.
Ascites commonly tend to occur in chronic rather than acute liver disorders. It results from portal hypertension due to severe liver scarring, alcohol ingestion, viral hepatitis, and obstruction of the hepatic vein. Nephrotic syndrome occurs when the kidney damage leads to protein leakage into the urine, resulting in this disease due to oncotic pressure.
While acute pancreatitis causes fluid accumulation in response to inflammation, chronic pancreatitis results in malnourishment, leading to loss of total body protein, ascites, and loss of oncotic pressure. Pancreatic cancer triggers direct fluid loss.
Direct Irritation
Peritoneum’s direct irritation causes fluid leakage as part of inflammation due to cancer or infection. Further, diseases of the ovary are also linked to ascites. Ovarian cancer has no initial symptoms, but ascites can signal its development.
Ovarian Disease
Meigs syndrome, which is an ovarian disease, causes a fibroma or benign tumor that leads to pleural effusion and resulting ascites. Hard surfaces of such an ovarian cyst can irritate the peritoneum, causing fluid leakage.
In rare cases, the disorder can also be the result of low thyroid function or hypothyroidism. Generally, this symptom manifests if the underactive thyroid has been left untreated for long. When thyroid levels return to normal, ascites is resolved.
How Ascites Develops in Liver Disorders
In those facing liver disorders, ascites results from the fluid leakage from the liver surface and intestine accumulating within the abs. A plethora of factors are responsible for this. This condition includes portal hypertension, kidney fluid retention, and hormone and chemical alteration, causing body fluid change. Albumin further leaks into the abs from blood vessels and fails to prevent fluid from leaking out as well. This condition is what causes ascites.
Signs and Symptoms
Cirrhosis is a liver disease complication involving liver cell loss and scarring and can signal ascites. When the condition is due to liver disease, gastroenterologists and hepatologists can be called in. Other specialists can care for the patient, depending on the cause of ascites.
Types of Ascites
Ascites is differentiated into two different types, exudative and transudative. This classification is associated with the protein in the fluid. A more useful system developed based on the amount of albumin found in the fluid in ascites, in comparison to serum albumin, is called SAAG/Serum Ascites Albumin Gradient. Further, ascites linked to portal hypertension is generally caused by cirrhosis, Budd-Chiari, or congestive heart failure and is higher than 1.1. Otherwise, this condition caused by reasons like malignancy and pancreatitis is less than 1.1.
Risk Factors
When greater than 25 ml buildup of fluid is within the abs, ascites results. Ascites causes liver functioning to stop. When your liver does not function well, the liquid comes in between the space of the abdominal organs and the lining. The 2010 guidelines in the Journal of Hepatology state that the 2-year survival rate is 50%. If ascites symptoms are experienced, consult your doctor immediately. Ascites is generally caused by liver scarring.
Therefore, the single most significant risk factor for ascites is liver damage. Some liver damage causes can range across cirrhosis, hepatitis C or B, history of alcohol usage. Other conditions triggering the risk for ascites include heart or kidney disease, pancreatic failure, liver, ovarian, endometrial, or pancreatic cancer. TB and hypothyroidism are also potential risk factors.
Symptoms & Picture
Ascites symptoms emerge gradually or at once, depending on the reason for the fluid aggregation. Symptoms don’t always mean there is an emergency. But do consult your doctor if you experience swollen or distended abs, immediate weight gain, breathlessness while lying down, loss of appetite, pain in the abs, heartburn, nausea, vomiting, and bloating.
Other conditions can cause ascites symptoms. Diagnosing the disorder requires a lot of steps. First, the doctor will check for abdominal swelling. Then, imaging/other testing methods will look for fluid buildup. These include the CT scan, ultrasound, MRI, blood tests, laparoscopy, and angiography.
There is a difference between patients developing ascites because of cirrhosis and because of cancer-induced peritoneum inflammation. Liver disease is generally painless. In cancer patients, ascites is more painful.
Apart from this, the symptoms are similar for both. First and foremost, there is an abdominal swelling which results due to the bid by the abdominal cavity to accommodate excess fluid. This process makes it tougher for the diaphragm to support breathing. This reason is why ascites is accompanied by breathlessness.
While a bloated abdomen with fluid can be easily recognized, ascites fluid amount may be small and tough to detect. As liquid rises, the patient will complain of heaviness or fullness in the abs, which could indicate the underlying medical condition triggering the ascites.
In liver cirrhosis, the fluid accumulates in the abdominal cavity, but there could be easy bruising, swelling, breast enlargement, and confusion induced by encephalopathy. If the ascites is caused by heart failure, edema and breathlessness are the key symptoms. In patients suffering from ascites due to heart problems, lying flat can trigger worse breathlessness along with the activity. This condition causes orthopnea. Further, ascitic patients with heart failure wake up in the middle of the night, facing paroxysmal nocturnal dyspnea. Patients suffering from cancer-linked ascites can experience abdominal swelling, along with pain, fatigue, and weight loss.
Those facing spontaneous bacterial peritonitis develop a fever and abdominal pain, when they have this disorder. This condition has symptoms that are associated with a lot of pain, nausea, appetite loss, tiredness, and breathlessness. There can be constipation and urinary urgency, too.
Besides this, fluid retention leads to pressure on internal organs resulting in discomfort. Ascites can also trigger bloating, back pain, and abdominal aches. The person can find it tough even to sit or walk.
Treatment and Management of Ascites
Treatment for ascites depends on what leads to the condition. Here are the simple lines of treatment and management.
Diuretics
Diuretics can treat ascites. Such drugs raise the salt and water, leaving the body, reducing pressure within the liver veins. When a patient is on diuretics, doctors may monitor his/her blood chemical makeup. Salt and alcohol use will have to be limited.
Paracentesis
In this process, a long, thin needle removes the extra fluid. It is injected into the abdominal cavity, through the dermal layer of the skin. As this method involves a risk of infection, patients may be given antibiotics. This is a standard treatment when ascites recurs or is severe, as diuretics don’t always work in late-stage cases.
A paracentesis may also be repeated, depending on the severity of the condition. Complications linked to paracentesis include infection, electrolyte disturbance, bleeding, and organ perforation. However, in extreme cases of this condition, the benefits can outweigh the pitfalls.
TIPS
This stands for a transjugular intrahepatic portosystemic shunt. TIPS diverts fluid from the portal vein to the central circulatory system, decreasing pressure in the liver and reducing ascites formation. Interventional radiology may include threading a stent or catheter under the skin from the internal jugular to the hepatic vein. This operation requires sedation.
Dual Treatments
Patients with cirrhosis and ascites can be ideal candidates for a potential liver transplant. Those with this condition and cancer may need paracentesis, with catheter drainage as diet and diuretics are not that effective. The patient does not have to go through repeated procedures. For cancer patients who don’t respond to paracentesis, peritoneovenoys shunts may be placed, mainly when TIPS has been carried out, or there are refractory ascites or a liver transplant. Further, for cirrhosis patients, alcohol must be limited and acetaminophen medicines minimized, as they require liver metabolism.
Surgery
In severe cases, a permanent rerouting tube is implanted in the body. Called the shunt, it regulates blood flow around the liver. The doctor may also recommend a liver transplant if ascites does not respond. This occurs when there is advanced liver disease.
Complications can develop. Spontaneous bacterial peritonitis can take place. Here, the fluid of the ascites buildup is infected. People may experience tenderness of the abs and abdominal discomfort, besides fever and lack of good health. They may also become tired, disoriented, and confused. If left untreated, this infection can be life-threatening. Antibiotics are critical for survival.
How is Ascites Diagnosed?
Sometimes imaging tests like ultrasonography may be carried out. Analysis of ascitic fluid can also occur. When the abdomen is tapped, the liquid gives off a particular sound. Tapping makes a hollow sound if the ab is enlarged with gas. Doctors cannot generally use a physical exam to detect the fluid until the volume is a quart or higher.
If the doctor is unsure if ascites is present or not, he/she may carry out computed tomography or ultrasonography. Along with this, a small sample of ascitic fluid can be easily taken by using a needle in what is called diagnostic paracentesis. Lab analysis of fluid buildup can distinguish the cause of this condition.
Complications linked to this condition include abdominal pain, water in the lung or pleural effusion, hernias, bacterial infections, and progressive kidney failure, also called hepatorenal syndrome.
Ascites cannot be prevented. But protecting your liver by adopting healthy habits can lower the risk. Always drink alcohol in moderation. Get hepatitis B vaccination. Also, ensure you avoid sharing needles or engaging in unprotected sex. Know the potential side effects of medicines, and if liver damage is one of them, talk to your doctor.
The most common reason for ascites is a cirrhotic liver. Risk factors also include alcohol abuse, viral hepatitis, congestive heart failure, kidney disease, and malignancy.
The diagnosis of this condition involves a physical exam, along with a detailed medical history. If ascites fluid is higher than 500 milliliters, a physical exam can reveal this condition. Additionally, smaller fluid amounts may be detected through an abdominal ultrasound. This disorder is also found through an ultrasound or CT scan.
Doctors generally focus on what caused the ascites. In this context, blood tests can detect reasons. Metabolic panels can detect liver injury patterns, electrolyte levels, and functional status od the kidney or liver. A complete blood count is also essential to assess the underlying conditions. Clotting or coagulation abnormalities can be the result of liver problems and lack of clotting proteins.
It can be that the underlying cause of ascites is not determined, based on history, exam, lab data, or imaging tests alone. In such cases, diagnostic paracentesis may be conducted, whereby the needle is injected to withdraw fluid for quicker analysis. For the diagnostic reasons, a small amount is enough; Larger volumes may be drawn if symptom relief from ascites is also sought.
The analysis involves sending collected fluid to the lab to post the drainage. The erythrocyte and leukocyte count, besides the albumin, level culture, and gram stain may be analyzed. Total protein, cytology, glucose, and amylase levels may also be considered. The results are analyzed for further evaluation and assessment of the possible causes of this condition.
Line of Treatment
The line of treatment for ascites is a diet that is low in sodium. In case the food is ineffective, drugs called diuretics may then be given. This type of drug includes spironolactone and furosemide. Due to diuretics, kidneys excrete additional sodium and water within the urine. This triggers frequent urination. If ascites makes breathing or eating tough, paracentesis may be recommended. Loss of albumin means the ascites patient may have to be given the albumin intravenously. In case large fluid amounts accumulate or other treatments don’t work, portosystemic shunts or a liver transplant may be recommended.
The shunt essentially connects the branch of or the portal vein to the general circulation vein, bypassing the liver. However, shunt placement is a surgical procedure that is invasive and can trigger deterioration of liver function, or brain function through hepatic encephalopathy. In case spontaneous bacterial peritonitis is detected, antibiotics like cefotaxime can work. As infection recurs in a year, norfloxacin or other medicines may then be prescribed.
If liver cirrhosis is causing ascites, patients should take water tablets and reduce salt. Water tablets prevent fluid retention. Certain ascites types are resistant to diuretics. In such cases, liver transplants can work best. Other treatments include paracentesis discussed earlier. When ascites is cancer-induced, shunts can be placed to move the abdominal fluid into the bloodstream. Chemo can be administered through the gastric tube in this case to stop fluid accumulation.
Ascites is linked to GI issues and reduced life expectancy. So treatment and management are critical for prolonging life. Physical exams to assess fluid buildup can examine body fat and abdominal circumference. Blood tests can determine the functioning of the liver and kidney. Further, fluid sample analysis can be used to check if cancer cells are present or infection is causing fluid leakage. Abdominal ultrasound can unearth underlying ascites causes. In case the ultrasound does not reveal the ascites cause, doctors can recommend MRIs. X-rays also serve as excellent imaging tools for diagnosis, confirming the buildup of lung fluid, metastasis of cancer, or heart failure.
In general, abdominal inflammation for any cause requires medical care. Fever and abdominal pain should be a signal or warning to consult the doctor immediately. Sometimes, physical exams are not enough. A complete blood count checks the elevated white blood cell count, anemia, and platelet count for liver functioning. Different blood tests can show asses kidney and liver functioning, protein in the body, and electrolyte balance.
If new onset of ascites results, paracentesis is recommended to obtain fluid for sample analysis. Gastroenterologists can also measure blood albumin levels concerning the amount found in the ascitic fluid to classify ascites types and diagnosis. When the protein is higher than the serum, the cause can be liver problems, heart failure, ovarian cancer, malnutrition, pancreatitis, or Budd-Chiari syndrome. When ascites protein is lower, certain malignancies and infections can occur.
Lab tests on the ascitic fluid include evaluation for electrolyte infection and assessment, besides an understanding of other substances.
Excess fluid in the abdominal hole causes shortness of breath and discomfort, depending on the seriousness of the condition. The treatment method is based on the reason for ascites aggregation, how fast the fluid has accumulated, is it a repetitive event or a first occurrence, and how do the symptoms impact the patient.
For those suffering from advanced liver cirrhosis, the focus is first on reducing the excess fluid and salts. Salt retention may be treated through metolazone/zaroxolyn and Lasix/furosemide. This treatment controls ascites fluid in numerous patients. Bodyweight is a measure of ascites control. The aim of diuretic therapy is losing 1-2 pounds of pressure per day, based on underlying medical issues. Once the ascitic fluid is drained, the medication is individualized to meet patient needs. Low serum sodium or hyponatremia may signal water restriction.
Prognosis
Alcohol abuse remains the most straightforward cause of ascites to treat. Those patients who develop ascites from cirrhosis have a 50% chance of dying within three years. Those with refractory ascites have a one-year mortality rate at 50%.
Outlook and prognosis of the disease depend on the underlying condition. Symptoms should be reduced, provided the cause is detected. If liver cirrhosis or diuretics resistant ascites results, paracentesis, and shunts can improve long-term life expectancy.
FAQs
What does the treatment of ascites involve?
The treatment depends mainly on the cause. Peritoneal carcinomatosis or malignant ascites can be cured through surgical resection of cancer or chemotherapy. Management of ascites about heart failure involves treatment through medical management and dietary limitations.
Is there a diet for ascites?
Managing ascites involves limited sodium intake. Water pills may also be prescribed. Sodium intake is generally restricted to less than 2 grams per day. It is widely recommended for ascites patients. In many cases, the approach needs to be combined with the use of diuretics, as restricting salt alone is not enough.
What medicines should be taken for ascites?
Diuretics raise salt and water excretion from kidneys. Recommended diuretics for setting liver induced ascites require a combination of Lasix and Furosemidein, a single daily dose of 40 and 100 mg, respectively. This can be increased to a maximum of 160 and 400 mg respectively, as long as no side effects are noted with medicines. Taking medicines in the morning is recommended to prevent nighttime urination.
For patients who cannot use medicines effectively, paracentesis may be required. 4-5 liters of fluid can be safely removed through this procedure at a time. For malignant ascites, the process is more effective than diuretic use.
Is surgery needed for ascites?
Surgical procedures may only be required in cases of refractory ascites. TIPS may be carried out by an interventionist radiologist under local anesthesia. The shunt is placed between the portal venous and systemic venous systems. This lowers portal pressure. This procedure works well for those not responding to aggressive medical treatments. It reduces ascites and eliminates the need for diuretics. However, complications can include brain damage or death. Traditional shut placements like systemic portosystemic and peritoneovenous shunts have been left aside due to high complication rates.
A liver transplant may be considered for advanced cirrhosis induced ascites. Liver transplant is a prolonged process requiring close monitoring and transplant specialist management.